Treatments for PD: Deep Brain Stimulation
We already know that not all PD patients are eligible for Deep Brain Stimulation and that it appears to be effective for some but not all of the people who do receive the treatment. DBS is used in some advanced stages of PD that do not respond well to meds in order to reduce tremors and involuntary movement. It is used in younger and older patients alike. According to CNN, more that 35,000 people have undergone the procedure worldwide. According to one study when successful, DBS a 71% showed an increase in "on" time to about 4.6 hours. In that study about 40% of the patients demonstrated some adverse affects.
Deep brain stimulation (DBS) is a surgical procedure which consists of implanting high frequency electrodes in the subthalmic nucleus (movement center) in order to stimulate neurons to produce brain-derived neurotrophic factor (BDNF) through an implanted pacemaker-like device. Essentially the surgery when successful interrupts the faulty signals of dopamine cell loss. It targets the subthalmic nucleus, thalmus or globus pallidus as predetermined through an MRI or CT. The result is that many Parkinson's patients who receive the treatment find that they require less medication for the PD symptoms they have. The PD treatment is given unilaterally to many patients, bilaterally to others. Some opt for one side only to determine who it will work for them.
The complicated procedure is not without its negative side effects in some cases. There have been neuro-cognitive changes even when there is improvement in motor function. Depression, falls, gait disturbance, motor dysfunction, dystonia, balance and cardiac issues are also side effects in some patients. Sometimes there are infections at the pacemaker site which is usually in the chest. These symptoms may depend upon where the electrodes are placed. If Optogenics is developed to the point of state of the art for PD and use in DBS, we will certainly see far more precision in the placement of the electrodes.
The procedure itself occurs under local anesthetic so that the patient can be awake. The patient's head is immobilized in a frame and an MRI is done to pinpoint where the electrode is to be implanted. Two incisions are made in the skull and the microelectrode is passed into the brain. Current is passed through the electrode and increased while the patients responds to questions and performs certain movement tasks. After trial and error, the correct location is determined and the permanent electrode is placed and secured. The hospital stay is usually a few days.
After the swelling has subsided usually about a week later, the neurostimulator wires are connected to the electrodes. The pacemaker is placed usually in the chest. It may be another two to four weeks before it is turned on. In theory the patients can control the current flow through the pacemaker which is usually implanted in the patient's chest. In actuality the patient meets with the neurologist several times for stimulator adjustment.
The stimulation can be adjusted or turned off unlike the thalamotomy which Michael J Fox underwent seven years after his diagnosis, DBS is reversible in that it can be turned off or adjusted as in cases where tremors recur. When sucessful, the results of DBS can be a radical and remarkable change.
DBS is being used as an alternative therapy to thalamotony and pallidotomy which are permanent irreversible surgical procedures, It is used for control of PD tremor and control of essential tremor. It is being investigated for primary dystonia (involuntary muscle contractions) as well as for intractable epilepsy, cluster headaches which are usually vascular and associated with high blood pressure, chronic intractable pain, morbid obesity and obsessive-compulsive behavior (OCD)
One thng that is important to remember if you are considering Deep Brain Surgery is the Neurosurgical Team that will be performing the surgery. Don't be afraid to ask those questions about their experience and track record. Patients need to be proactive about their treatments.
DBS is not an inexpensive surgery. Costs can vary from $50,000 to $120,000 although in many cases are covered by Medicare and private insurance. Nonetheless, the co-pay can be very high.
In most clinical trials, patients with atypical symptoms, surgical contraindications such as MRIs or past PD surgery are excluded. Most studies will take both genders up to 75 or 80 years of age. What is necessary is that patients must fully disclose their medical history which includes psychiatric history; a desire for the surgery without full disclosure can lead to unexpected side effects.
So who does DBS work for or rather why does it work? How are the cells calmed or stimulated by the electrical shocks they receive? That still isn't clear but researchers in Scotland are exploring the idea that by stimulating other areas perhaps they can affect postural symptoms and gait issues also. One thing that is known is that when successful, DBS can improve the quality of life for the recipient.
Addendum:
On April of 2009, 50 DBS experts assembled to share experiences with Deep Brain Surgery procedures. They reached a consensus, per a recent news release issued by the UCLA Los Angeles Newsroom on October 10, 2010.
The findings include the best candidates for DBS; the importance of having an experienced team with an expertise in stereotactic neurosurgery performing the surgery. For some patients, DBS can be used for patients who have had PD surgeries. It is important to remember that certain treatments of the subthalmic nuclei can increase depression. And a reminder that surgery has complications with infection ranking highest.
You can read the full news release at the UCLA website.
References:
The first link is for DBS clinical trials - both closed and recruiting.
VIDEOS about DBS
You can watch video clips for PPN, dystonia and tremor.
And have your choice of many clips at YouTube.
If you live in Norway, there is a DBS clinical trial currently recruiting:
Clinical trial BCT00855621
Contact: Dr Mathias Toft 4799514189
Open to: 18-75 years
Gender: both
To study motor function, quality of life and cognitive function
Who is a good candidate for Deep Brain Stimulation
The medical history of DBS
Coming next:
Spinal Cord Stimulation
Optogenics
Magnetic Stimulation
Showing posts sorted by relevance for query deep brain stimulation. Sort by date Show all posts
Showing posts sorted by relevance for query deep brain stimulation. Sort by date Show all posts
Wednesday, March 25, 2009
Friday, March 20, 2009
Brain Stimulation Breakthrough for Parkinson's Disease
Possible PD treatment without risky surgery
 Today I've been reading a fascinating article in the New York Times about a recent new approach to treating Parkinson's disease. It describes spinal cord stimulation in dopamine-deprived rats where a mild electrical current flows up the rodent's spinal cord and into the brain. As long as that current is maintained the rodents regain their ability to move normally.
Today I've been reading a fascinating article in the New York Times about a recent new approach to treating Parkinson's disease. It describes spinal cord stimulation in dopamine-deprived rats where a mild electrical current flows up the rodent's spinal cord and into the brain. As long as that current is maintained the rodents regain their ability to move normally.
This procedure in being tested in monkeys now because humans and monkeys are the only two species which get PD naturally. If it is proven to be safe and efficient, spinal cord stimulation will be a potential alternative to DBS since it requires no risky invasive surgery to plant electrodes deep in the brain. It may be effective for some of the 70% of severely impaired PDers who do not qualify for deep brain stimulation.
This could represent a major paradigm shift in available treatments. It is not without drawbacks-tradeoffs, however since one side effect is reported to be a never-ending mini-vibration described by Dr Ali Rezai, director of the Cleveland Clinic Center for Neurological Restoration as "pins and needles."
Read more:
http://www.nytimes.com/2009/03/20/health/20spinal.html?_r=1&ref=health
 Today I've been reading a fascinating article in the New York Times about a recent new approach to treating Parkinson's disease. It describes spinal cord stimulation in dopamine-deprived rats where a mild electrical current flows up the rodent's spinal cord and into the brain. As long as that current is maintained the rodents regain their ability to move normally.
Today I've been reading a fascinating article in the New York Times about a recent new approach to treating Parkinson's disease. It describes spinal cord stimulation in dopamine-deprived rats where a mild electrical current flows up the rodent's spinal cord and into the brain. As long as that current is maintained the rodents regain their ability to move normally.This procedure in being tested in monkeys now because humans and monkeys are the only two species which get PD naturally. If it is proven to be safe and efficient, spinal cord stimulation will be a potential alternative to DBS since it requires no risky invasive surgery to plant electrodes deep in the brain. It may be effective for some of the 70% of severely impaired PDers who do not qualify for deep brain stimulation.
This could represent a major paradigm shift in available treatments. It is not without drawbacks-tradeoffs, however since one side effect is reported to be a never-ending mini-vibration described by Dr Ali Rezai, director of the Cleveland Clinic Center for Neurological Restoration as "pins and needles."
Read more:
http://www.nytimes.com/2009/03/20/health/20spinal.html?_r=1&ref=health
Thursday, March 26, 2009
Parkinson's Blue Light District
Optogenics and the G-protein coupled receptor - what will it mean for PD?
 It all begins in the brain, that complicated computer which processes analyzes, sorts, stores, and relays electrical impulses to keep the body functioning as designed. Sometimes, however, things go wrong, small parts malfunction, current varies to affect operation and the body human begins to get error messages. On many occasions we reboot, clean up some programs, add a program and we're good to go. Or we call IT or MIS and those specialists can fix many problems. But at other times the error messages persist.
It all begins in the brain, that complicated computer which processes analyzes, sorts, stores, and relays electrical impulses to keep the body functioning as designed. Sometimes, however, things go wrong, small parts malfunction, current varies to affect operation and the body human begins to get error messages. On many occasions we reboot, clean up some programs, add a program and we're good to go. Or we call IT or MIS and those specialists can fix many problems. But at other times the error messages persist.
Parkinson's disease sends some of those errors messages. The specialists here have been able to take patients to the edge of state of the art with medications which abate progression, which go to the source to make some symptoms ease or stop for awhile, but the disease remains. New treatments were developed to control the symptoms by interrupting the error messages. From radical surgery to invasive but less radical surgery, some patients have found relief while others were the same or worse.
We already know that not all PD patients are eligible for Deep Brain Stimulation (DBS) and that it appears to be effective for some but not all of the people who do receive the treatment. Ongoing research in an area called optogenics may become a way to change some of that situation by employing a method which allows for more precision in the surgical procedure by prior identification of the neurons which would benefit from stimulation. Basically the focus become tighter and more accurate before the nodes are set. One goal is to improve the results of DBS.
While aspects of the area of science now called Optogenics have existed for several years, the older apects are now being combined with a method developed in Karl Deisseroth's lab. By inserting a small fiberoptic cable into the brain the light impulses can be controlled as they search for the affected neurons. This procedure allows for smaller and smaller targets of the G-protein on the specific neuron.
have existed for several years, the older apects are now being combined with a method developed in Karl Deisseroth's lab. By inserting a small fiberoptic cable into the brain the light impulses can be controlled as they search for the affected neurons. This procedure allows for smaller and smaller targets of the G-protein on the specific neuron.
The current procedures were developed by under the direction of Karl Deisseroth, MD, PhD at Stanford University. The project required the work of bioengineering and medical neuroscience and neurology students and faculty as they explored target after target to finally find that stimulation of the axons that connect the subthalmic nucleus are actually in areas closer to the brain's surface. While treatments would be still invasive, they would be less invasive thanks to better targeting at the G protein coupled receptors at the cell surface.
 At Stanford University scientists were able to incorporate the technique in model mouse brains to produce activity in a real-time frame using both blue light to signal activity and yellow light to stop. The cells returned to their normal status unchanged at completion.
At Stanford University scientists were able to incorporate the technique in model mouse brains to produce activity in a real-time frame using both blue light to signal activity and yellow light to stop. The cells returned to their normal status unchanged at completion.
An interesting thing about neurons is that they communicate in a manner similar to binary code. Sometimes on sometimes off similar to the 0s and 1s of binary code. By being able to communicate in their on-off patterns, learning the neuron language might enable direct actual neural instruction through the flashing of the blue and yellow lights. In another metaphor, Optogenics appears to be the cell tower, now what is needed is a phonebook.
Optogenics holds hope for spinal cord injuries, restoring function to paralyzed limbs, allowing for new therapies, closely targeted pharmaecuticals and possibly become a neuronal therapy in itself.
Optogenics: A process by which brain cells can be activated by specific light
Channel Rhodopsins (ChR): light-activated ion channels appear to be coupled with the photoreceptor so that they do not require chemical signalling but instead are triggered by light.
Channel Rhodopsin (ChR2): algae-derived gene protein which makes neurons more active upon blue light exposure. Currently vector-introduced to the desired neurons. This is the "emit a signal" protein
Halo-rhodopsin (NpHR): from a microbe which can make neurons less active. The instruction here is to "stop emitting." They respond to yellow light.
G protein coupled receptors (GPCRs): signalling proteins found on the surface of nearly all cells.
Reading List:
http://storybank.stanford.edu/stories/controlling-brain-with-optogenics
http://www.newscientist.com/article/dn16807
http://www.freepatentsonline.com/7488583.html
http://pubs.acs.org/cen/science/86/8612sci1.html
http://www2.hu-berlin.de/biologie/expbp/Homepage-new_10408.pdf
http://web.mit.edu/newsoffice/2007/brain-block.html
http://med.stanford.edu/news_releases/2009/march/deisseroth.html
http://storybank.stanford.edu/stories/neural-traffic-light-a-go-better-brain-research
http://www.medicalnewstoday.com/articles/143132.php
Targeting the Brain's GO pathway - 2010 It all begins in the brain, that complicated computer which processes analyzes, sorts, stores, and relays electrical impulses to keep the body functioning as designed. Sometimes, however, things go wrong, small parts malfunction, current varies to affect operation and the body human begins to get error messages. On many occasions we reboot, clean up some programs, add a program and we're good to go. Or we call IT or MIS and those specialists can fix many problems. But at other times the error messages persist.
It all begins in the brain, that complicated computer which processes analyzes, sorts, stores, and relays electrical impulses to keep the body functioning as designed. Sometimes, however, things go wrong, small parts malfunction, current varies to affect operation and the body human begins to get error messages. On many occasions we reboot, clean up some programs, add a program and we're good to go. Or we call IT or MIS and those specialists can fix many problems. But at other times the error messages persist.Parkinson's disease sends some of those errors messages. The specialists here have been able to take patients to the edge of state of the art with medications which abate progression, which go to the source to make some symptoms ease or stop for awhile, but the disease remains. New treatments were developed to control the symptoms by interrupting the error messages. From radical surgery to invasive but less radical surgery, some patients have found relief while others were the same or worse.
We already know that not all PD patients are eligible for Deep Brain Stimulation (DBS) and that it appears to be effective for some but not all of the people who do receive the treatment. Ongoing research in an area called optogenics may become a way to change some of that situation by employing a method which allows for more precision in the surgical procedure by prior identification of the neurons which would benefit from stimulation. Basically the focus become tighter and more accurate before the nodes are set. One goal is to improve the results of DBS.
While aspects of the area of science now called Optogenics
 have existed for several years, the older apects are now being combined with a method developed in Karl Deisseroth's lab. By inserting a small fiberoptic cable into the brain the light impulses can be controlled as they search for the affected neurons. This procedure allows for smaller and smaller targets of the G-protein on the specific neuron.
have existed for several years, the older apects are now being combined with a method developed in Karl Deisseroth's lab. By inserting a small fiberoptic cable into the brain the light impulses can be controlled as they search for the affected neurons. This procedure allows for smaller and smaller targets of the G-protein on the specific neuron.The current procedures were developed by under the direction of Karl Deisseroth, MD, PhD at Stanford University. The project required the work of bioengineering and medical neuroscience and neurology students and faculty as they explored target after target to finally find that stimulation of the axons that connect the subthalmic nucleus are actually in areas closer to the brain's surface. While treatments would be still invasive, they would be less invasive thanks to better targeting at the G protein coupled receptors at the cell surface.
 At Stanford University scientists were able to incorporate the technique in model mouse brains to produce activity in a real-time frame using both blue light to signal activity and yellow light to stop. The cells returned to their normal status unchanged at completion.
At Stanford University scientists were able to incorporate the technique in model mouse brains to produce activity in a real-time frame using both blue light to signal activity and yellow light to stop. The cells returned to their normal status unchanged at completion.An interesting thing about neurons is that they communicate in a manner similar to binary code. Sometimes on sometimes off similar to the 0s and 1s of binary code. By being able to communicate in their on-off patterns, learning the neuron language might enable direct actual neural instruction through the flashing of the blue and yellow lights. In another metaphor, Optogenics appears to be the cell tower, now what is needed is a phonebook.
Optogenics holds hope for spinal cord injuries, restoring function to paralyzed limbs, allowing for new therapies, closely targeted pharmaecuticals and possibly become a neuronal therapy in itself.
Optogenics: A process by which brain cells can be activated by specific light
Channel Rhodopsins (ChR): light-activated ion channels appear to be coupled with the photoreceptor so that they do not require chemical signalling but instead are triggered by light.
Channel Rhodopsin (ChR2): algae-derived gene protein which makes neurons more active upon blue light exposure. Currently vector-introduced to the desired neurons. This is the "emit a signal" protein
Halo-rhodopsin (NpHR): from a microbe which can make neurons less active. The instruction here is to "stop emitting." They respond to yellow light.
G protein coupled receptors (GPCRs): signalling proteins found on the surface of nearly all cells.
Reading List:
http://storybank.stanford.edu/stories/controlling-brain-with-optogenics
http://www.newscientist.com/article/dn16807
http://www.freepatentsonline.com/7488583.html
http://pubs.acs.org/cen/science/86/8612sci1.html
http://www2.hu-berlin.de/biologie/expbp/Homepage-new_10408.pdf
http://web.mit.edu/newsoffice/2007/brain-block.html
http://med.stanford.edu/news_releases/2009/march/deisseroth.html
http://storybank.stanford.edu/stories/neural-traffic-light-a-go-better-brain-research
http://www.medicalnewstoday.com/articles/143132.php
In 2014 a small clinical trial for use of CBD oil for seizure disorders was published. It is referenced because of the explanation of the G-protein.
You can now find numerous optogenics studies.
You might also enjoy this article about Karl Deisseroth
2015 Optogenics study: Illuminating Parkinson's Therapy with Optogenics
Sunday, January 29, 2012
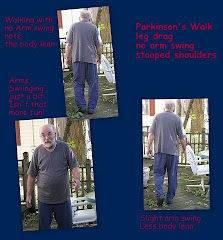
Postural Instability and Gait Disturbances in Parkinson's Disease
Steve had several PD precursor symptoms for years. Some motor symptoms appeared early but did not interfere with lifestyle. Postural Instability appeared about a year prior to his diagnosis. The appearance was subtle. He would climb a ladder to perform some honeydo chore and come back down saying that he felt uncomfortable, unsteady, not right about being on a ladder. And this was inside the house. He felt that the sensation was real - as his wife I had some doubts. He was right; I wish he'd been wrong. He was exhibiting one of the Big 4 Parkinson's symptoms.
What is Postural Instability? To my eyes it is the failure to be able to identify the vertical but really it is much more. It occurs when reflexes are unable to adjust or compensate for sway, vertical, horizontal and diagonal and environmental changes. Gait Disturbances such as freezing or the loss of the natural rhythms which initiate and maintain gait, the rhythm aids in turning and in stride length are interrupted or short circuited.
An easy way to identify how a PwP might sense the problem is to visualize a set of steps which do not conform to the normal rise and/or tread depth. Imagine (feel) walking up or down the stairs where the next step you take is not the same height difference as the previous step so that the spacing rhythm is disrupted. Perhaps one riser is the code max of 7.75" while another is 8" or 8.5". You automatically reach for the next step and it isn't where it is supposed to be. I've seen it when an amateur cuts a step stringer and it can kill you. Your body has a natural rhythm when descending or ascending a flight of stairs. You can simulate this by placing a magazine on one step, two on the next, none after that. You'll feel very disconcerted and off balance. You grab for the handrail. What should come naturally doesn't. That's just a part of Postural Instability and Gait Disturbance.
We recently received an email asking for information about a procedure known as ExAblate®. The writer wanted to know if there was hope for Parkinson's patients with Postural Instability after she had seen the Diane Sawyer segment on ABC World News in which a ET patient of Dr William Jeff Elias discussed her Essential Tremor life before and after this unique targeted laser procedure. Although there may be a genetic link between some cases of ET and some cases of PD, the targeting will be different.
ExAblate® is a procedure done using Magnetic Resonance guided Focused Ultrasound *MRgFUS) technology developed by a Swiss company, InSightec. Although there is a study underway for Parkinson's patients, it will only take place at the Center of Ultrasound Functional Neurosurgery in Solothurn, Switzerland. The studies being conducted by Dr William Jeff Elias in the US are directed to Essential Tremor as the specific brain targets have been identified.
The Parkinson's study by Insightec is geared towards long-term chronic, therapy-resistant movement disorders. Perhaps there will be some surprise results as Postural Instability (PI) or Postural Instability and Gait Disturbances (PIGD) are inadvertently addressed as well. We can only hope.
There is some research in progress. In 2009 the Michael J Fox Foundation awarded five research grants totaling $2 million for research addressing Postural Instability and Gait Disorders.
Over the last few years there has been research into a part of the brain stem known as the pedunculoponitine nucleus (PPN) which is a bi-lateral target for stimulation to address gait freezing. We plan to write more about it. The PPN processes sensory and behavioral data, is related to arousal, attention. learning, locomotion rewards and voluntary limb movement. While the PPN gets input from several areas of the brain, it sends but does not receive information from the substantia nigra pars compacta. Autposies of PD brains show degeneration of the pedunculopontine nucleus. Researchers identifed the PPN as a target for Deep Brain Stimulation and the first PPN DBS surgeries have shown promise. The point is that the PPN seems to be very significant in Parkinson's disease.
While there don't seem to be medications which work effectively to address Postural Instability, there are some exercises which might help if done on a regular basis. We covered marching in place as a chair exercise a few years ago. Shoulder exercises are important for posture and range of motion. This week we'll post two more excellent exercises.
Cerebral blood flow changes induced by pedunculopontine nucleus stimulation in patients with advanced PD
Topical organization of the pedunculopontine nucleus by Christina Martiniz-Gonzalez, J Paul Bolan and Juan Mena-Segovia from the Medical Research Council Anatomical Neuropharmacology Unit, Dept of Pharmaacology, University of Oxford, Oxford, UK
Sunday, May 10, 2009
Forced Exercise to Relieve Parkinson's Disease Symptoms
I'm Pedaling as Fast as I Can
In 2003 Cleveland Clinic biomedical engineer Jay Alberts, PhD was on a 480 mile tandem bike trip across the state of Iowa with his friend Kathy who was a PWP (person with Parkinson's) Normally she would pedal at 50-60 rpm, but during this trip with Dr. Alberts she had to pedal at 80-90 RPM. Although the pedaling muscle was provided by Dr Alberts, Kathy's legs moved with the pedals at the speed which he set. When they had gone half the distance they noticed that Kathy's hand tremors had stopped.
Intrigued by Kathy's improvement in motor skills Dr Alberts experimented with another Parkinsons patient in 2006. This patient's symptoms were controlled by an electronic device that had been inserted in his brain by DBS surgery. He rode on the tandem bike with Dr. Alberts for 50 miles with the device turned off. He too exhibited no symptoms during the trip.
This discovery led Dr. Alberts to research Assisted Tandem Bicycle riding based upon his biking and his previous experiences with animal studies. It's called Forced Exercise. "The idea behind it is if we force them to pedal at a higher rate, this allows them to have biochemical changes that are necessary for improvements in motor function," explains Dr. Jay Alberts. "There's a possibility that there's an increase in dopamine or there's an increase in these neuro growth factors."
In a subsequent study with the a voluntary exercise control on a stationary bike or the forced exercise on a tandem bike with a trainer, an improvement of about 30% was measured in the forced exercise group. The improvements declined to 20% about two weeks after the study ended. This suggests the need for regular ongoing forced exercise as a significant part of exercise therapy.
While patients on medication and with deep brain stimulation show a significant improvement with these aids, if the meds are stopped or the DBS is turned off, the patient becomes symptomatic very rapidly. With therapeutic forced exercise, the improvements taper gradually. Dr Alberts feels that the therapies might work well together. By pushing the cyclist past his/her comfort zone by exercising the lower half of the body, the upper half improves. Whether this is a needed stimulus to the central nervous system is still unknown but the goal is to be as symptom free as possible and without the need for medication.
So if the study shows this to be a viable treatment a patient could ride a tandem bike with a friend or family member or use an electric motor driven stationary bike. Because most Parkinson's people cannot pedal at 80-90 rpm, the additional boost to get the leg stimulation comes from either the tandem companion rider or the motor of the stationary bicycle.
I'm hoping that I can convince the Therapy Center to buy a motor driven bike.
references and resources:
Theracycle
Kent State University Magazine summer 2009
ReckMotoMed Website
WNDU.com May 10, 2009
Pedaling to Beat Parkinsons
How You Can Help One Man's Challenge
http://www.lerner.ccf.org/news/documents/LRIMagazineFINAL.pdf
August 4, 2009 Thought you'd like an update
Forced Exercise Appears to Produce Benefits Similar to Levadopa
2011 Addendum:
See PD Trials for contact information about the Dr Albert's Forced Exercise trial, The Therapeutic Effect of Exercise on Parkinson's disease, Study ID: 09-439
2012 Addendum
In 2003 Cleveland Clinic biomedical engineer Jay Alberts, PhD was on a 480 mile tandem bike trip across the state of Iowa with his friend Kathy who was a PWP (person with Parkinson's) Normally she would pedal at 50-60 rpm, but during this trip with Dr. Alberts she had to pedal at 80-90 RPM. Although the pedaling muscle was provided by Dr Alberts, Kathy's legs moved with the pedals at the speed which he set. When they had gone half the distance they noticed that Kathy's hand tremors had stopped.
Intrigued by Kathy's improvement in motor skills Dr Alberts experimented with another Parkinsons patient in 2006. This patient's symptoms were controlled by an electronic device that had been inserted in his brain by DBS surgery. He rode on the tandem bike with Dr. Alberts for 50 miles with the device turned off. He too exhibited no symptoms during the trip.
This discovery led Dr. Alberts to research Assisted Tandem Bicycle riding based upon his biking and his previous experiences with animal studies. It's called Forced Exercise. "The idea behind it is if we force them to pedal at a higher rate, this allows them to have biochemical changes that are necessary for improvements in motor function," explains Dr. Jay Alberts. "There's a possibility that there's an increase in dopamine or there's an increase in these neuro growth factors."
In a subsequent study with the a voluntary exercise control on a stationary bike or the forced exercise on a tandem bike with a trainer, an improvement of about 30% was measured in the forced exercise group. The improvements declined to 20% about two weeks after the study ended. This suggests the need for regular ongoing forced exercise as a significant part of exercise therapy.
While patients on medication and with deep brain stimulation show a significant improvement with these aids, if the meds are stopped or the DBS is turned off, the patient becomes symptomatic very rapidly. With therapeutic forced exercise, the improvements taper gradually. Dr Alberts feels that the therapies might work well together. By pushing the cyclist past his/her comfort zone by exercising the lower half of the body, the upper half improves. Whether this is a needed stimulus to the central nervous system is still unknown but the goal is to be as symptom free as possible and without the need for medication.
So if the study shows this to be a viable treatment a patient could ride a tandem bike with a friend or family member or use an electric motor driven stationary bike. Because most Parkinson's people cannot pedal at 80-90 rpm, the additional boost to get the leg stimulation comes from either the tandem companion rider or the motor of the stationary bicycle.
I'm hoping that I can convince the Therapy Center to buy a motor driven bike.
references and resources:
Theracycle
Kent State University Magazine summer 2009
ReckMotoMed Website
WNDU.com May 10, 2009
Pedaling to Beat Parkinsons
How You Can Help One Man's Challenge
http://www.lerner.ccf.org/news/documents/LRIMagazineFINAL.pdf
August 4, 2009 Thought you'd like an update
Forced Exercise Appears to Produce Benefits Similar to Levadopa
2011 Addendum:
See PD Trials for contact information about the Dr Albert's Forced Exercise trial, The Therapeutic Effect of Exercise on Parkinson's disease, Study ID: 09-439
2012 Addendum
Forced Exercise and Parkinson's Disease a significant article by Jay Alberts, Susan Linder, Amanda Penko, Mark Lowe and Michael Phillips
Friday, December 11, 2009
Treatments for Parkinson's Disease
Parkinson's disease is treated in several ways. And treatment is what is currently available; there are no sure-fire cures. Sadly, treatments often lose their effectiveness to combat both the symptoms and the progression of the disease as the years pass.
To confound the problem of treatment is the fact that Parkinson's disease is a collection of syndromes with varied symptoms and progression rates. Treatment needs to be adjusted to the individual.
To confound the problem of treatment is the fact that Parkinson's disease is a collection of syndromes with varied symptoms and progression rates. Treatment needs to be adjusted to the individual.
Knowledgeable physicians and proactive PD patients learn to be aware of when adjustments in dosage, timing, the addition of another medication to work with the current prescribed med can be effective in prolonging "on" times and reducing "off" times. And some are aware that nutritional supplements are as much a part of a therapeutic regimen as the prescription pad. Other physical therapies are acknowledged by advanced medical plans so that all you need is a prescription for a sessions which the patient can often continue.
So what are the options? Let's begin with a summary of prescribed medications by category. We'd love to post the handy-dandy medication chart we made listing product names, generic names, symptoms for use, contraindications, side effects and some general information about the way the medication works but, doggone it, we've been unable to transfer the table successfully to the blog-site. We're working on it. Today we're working from the printed version.
Prescription Medication:
DOPAMINERGICS are the most common - these have been the "gold standard" for many years but are not without problems and may not be the best choice for the newly diagnosed.
The standard treatment has been Sinemet (levodopa-carbidopa) This is still the first line treatment for the majority of patients but is losing some ground to Azilect
Levodopa is absorbed into the blood stream in the small intestine and converted into dopamine after in crosses the blood brain barrier. (note: dopamine cannot cross the blood brain barrier)
Levodopa is absorbed into the blood stream in the small intestine and converted into dopamine after in crosses the blood brain barrier. (note: dopamine cannot cross the blood brain barrier)
Problem: Levodopa has a short half-life and a major side effect is nausea which can last up to a year. A number of other problems can occur including hallucinations common to other PD meds.
The combination of levodopa-carbidopa improves the functioning of the levodopa, prolongs the "wearing off" meaning fewer side effects such as the dyskinesia-dystonia. It can also allow for a lower levodopa dosage.
Other dopaminergics include Madopar which is levodopa-benserazide hcl.
Carbidopa is also a dopaminergic - it inhibits the peripheral metabolism of levodopa prior to crossing the BBB.
For people who have trouble swallowing there is Parcopa (levodopa-carbidopa) which is orally dissolvable.
The most common immediate unpleasant side effect of dopaminergics is nausea which can last for up to a year but may be relieved by increasing the carbidopa. Timing is important and taking with a low-protein meal may reduce nausea. It is suggested that a regular protein meal follow Sinemet by at least one hour.
DOPAMINE AGONISTS - bind to different dopamine receptors - they are sometimes taken with antagonists because they have a short half life. The binding activates the dopamine receptor pathways.
The combination of levodopa-carbidopa improves the functioning of the levodopa, prolongs the "wearing off" meaning fewer side effects such as the dyskinesia-dystonia. It can also allow for a lower levodopa dosage.
Other dopaminergics include Madopar which is levodopa-benserazide hcl.
Carbidopa is also a dopaminergic - it inhibits the peripheral metabolism of levodopa prior to crossing the BBB.
For people who have trouble swallowing there is Parcopa (levodopa-carbidopa) which is orally dissolvable.
The most common immediate unpleasant side effect of dopaminergics is nausea which can last for up to a year but may be relieved by increasing the carbidopa. Timing is important and taking with a low-protein meal may reduce nausea. It is suggested that a regular protein meal follow Sinemet by at least one hour.
DOPAMINE AGONISTS - bind to different dopamine receptors - they are sometimes taken with antagonists because they have a short half life. The binding activates the dopamine receptor pathways.
I'm not going to list all but the most common include bromocriptine, Requip XL (ropinirole), Mirapex, Trivastal, and the Neupro Transdermal patch (rotigotine) returned to the European market last June and is anticipated to return to the US market in July 2012 - although it is not entirely unavailable to US prescription holders.
DOPAMINE ANTAGONISTS are primarily used as anti-psychotics. They bind but they don't stimulate dopamine receptors - they copy the effect of DA.
COMT INHIBITORS - inhibit the catechol-menthyltransferase enzyme to inhibit the break-down of dopamine after its release in the brain. They begin to work immediately after the first dose. They are often combined with levodopa-carbidopa later in treatment. Common names include Comtan (entacapone) Tasmar (tolcapone and Stalevo (which is a combination of levodopa-carbidopa-entacapone)
MAOI-Bs are another category - Monoamine oxidase-B inhibitors or MAO-B inhibitors slow the breakdown of dopamine by inhibiting MAO-B enzyme. By this action, the dosage of levodopa-carbidopa may also be reduced.
DOPAMINE ANTAGONISTS are primarily used as anti-psychotics. They bind but they don't stimulate dopamine receptors - they copy the effect of DA.
COMT INHIBITORS - inhibit the catechol-menthyltransferase enzyme to inhibit the break-down of dopamine after its release in the brain. They begin to work immediately after the first dose. They are often combined with levodopa-carbidopa later in treatment. Common names include Comtan (entacapone) Tasmar (tolcapone and Stalevo (which is a combination of levodopa-carbidopa-entacapone)
MAOI-Bs are another category - Monoamine oxidase-B inhibitors or MAO-B inhibitors slow the breakdown of dopamine by inhibiting MAO-B enzyme. By this action, the dosage of levodopa-carbidopa may also be reduced.
Common MAOI-Bs include Selegiline or Eldepryl, Zelpar. These still carry the tyramine-cheese effect warning which is actually more common to MAO-As. There is also EMSAM which is a transdermal patch of Selegiline which is also approved by the FDA for treatment of Major Depressive Disorder. The 6 mg EMSAM patch does not carry a tyramine warning..
Another MAO-B which differs chemically from Selegiline is Azilect. Many people are turning to Azilect as a first line medication - before any other anti-parkinson's meds because it has shown to be very effective in slowing the progression of this disease. Currently there are trials to determine its effectiveness in being later combined with levodopa-carbidopa to reduce the "Off" times and to prolong the effective usage of levodopa/carbidopa. On December 14, 2009 FDA approved the removal of the tyramine warning from the Azilect label.
Another MAO-B which differs chemically from Selegiline is Azilect. Many people are turning to Azilect as a first line medication - before any other anti-parkinson's meds because it has shown to be very effective in slowing the progression of this disease. Currently there are trials to determine its effectiveness in being later combined with levodopa-carbidopa to reduce the "Off" times and to prolong the effective usage of levodopa/carbidopa. On December 14, 2009 FDA approved the removal of the tyramine warning from the Azilect label.
OTHER MEDS include off-label meds which have been effective for some people.
They include: Amantadine, an anti-viral which increases the release of dopamine.
DynaCirc CR - a calcium channel blocker or calcium agonist - which tries to restore the cells to a more youthful saline condition.
DynaCirc CR - a calcium channel blocker or calcium agonist - which tries to restore the cells to a more youthful saline condition.
Note: it is thought that dopamine is forced into the cytoplasm prematurely and there it combines with misfolded alpha synuclein and calcium to create the gummy mess which causes the dopamine to die.
The Exelon patch - a reversible chlorinesterase inhibitor used for moderate dementia, cognitive skills loss and executive skills.
The Exelon patch - a reversible chlorinesterase inhibitor used for moderate dementia, cognitive skills loss and executive skills.
Aricept functions in a similar way but is still more common to Alzheimer's patients.
In the next category are the ANTICHLORINERGICS which block acetylcholine to compensate for that loss of homeostasis with the declining dopamine neurons. They are not as commonly used now but are the oldest of the modern PD meds.
A few names are Artane, Cogentin, Norflex, Benadryl.
I'm not going to list the ANTI-DEPRESSANTS and the various categories such as SSRIs but that is another category of PD meds and yes, we have another fussy table that won't transfer properly. But we will post it one day because it is helpful.
Okay, what's next? Many people would love to be able to use NUTRITIONAL SUPPLEMENTS or alternatives to conventional medication and there are a number of important supplements, but make no mistake, they too have side effects and can have an impact upon brain/body homeostasis - often the reason for use - unless contraindicated or mis-used.

Most of these nutritional supplements can be found in foods but to get the right amounts to fight free radicals we supplement. To get the optimal amounts of some nutritional supplements, we take capsules and tablets, powders and liquids. Often we could not possibly eat enough of a particular food and/or those food may also include other elements which in larger amounts might not be so beneficial. Remember also that for PwPs smaller capsules seem to work best unless you can find a chewable or better yet a sublingual that doesn't result in a burning sensation.
In this category are Antioxidants such as CoQ10. Another very important antioxidant for PD is glutathione in either sublingual, liquid or the expensive IV treatment. We'll be writing more on glutathione and N-Acetyl L-Cysteine. Vitamins C and E are antioxidants which work synergistically, even more so with the addition of Alpha Lipoic Acid. Vitamin A is well stored in the body but an occasional boost might not hurt either as beta carotene or as Vitamin A.
PwPs have deficiencies of certain B vitamins. A low dose of B complex (25-50 mgs max) might be in order. Otherwise B2, B5, B6 and B12 can be adjusted separately.
D3 will help to boost the immune system and for PD patients who don't get out into the sunlight much - there is no other alternative to producing Vitamin D in the body. Other supplements to consider are: Acetyl L-Carnitine which is sometimes found in combination with Alpha Lipoic Acid.
Creatine is not just for weightlifters and body builders, PwPs are taking it also. Not just any creatine, however but micronized creatine monohydrate which is available as a pharmaceutical grade product. Creatine is also a powerful antioxidant for scavenging ROS.
Creatine is not just for weightlifters and body builders, PwPs are taking it also. Not just any creatine, however but micronized creatine monohydrate which is available as a pharmaceutical grade product. Creatine is also a powerful antioxidant for scavenging ROS.
You don't hear much discussion about mushroom extracts for PD immune system enhancers but Maitake, Reishi, Shitake and Astragalus can sometimes be found in a combination capsule (to keep the cost down).
For folks with digestive issues, consider ginger or Lactobaculis Acidophilus for a healthier GI tract balance. This is very important when diarrhea is an issue or after a course of antibiotics which also does a number on the friendly flora in the gut.
Omega 3 oil is another nutritional supplement. Another interesting source of essential fatty acids (EFAs) for PD is Coconut Oil, a medium chain triglyceride. It has an unique combination of fatty acids and does come in capsule form if you don't find one with a decent taste for food preparation.
If you're not drinking green tea, there's a capsule for that and might actually be better for providing what you need without what you do't need. And if you don't cook with a good turmeric from India, it also comes in pills as well. The primary ingredient of turmeric is a powerful anti-inflammatory in the form of curcuminoids. Recent research (2012) indicates that the curcuminoids in turmeric are effective in preventing the clumping of alpha synuclein proteins. Moreover, it may do this by speeding up the folding and reconfiguration of alpha synuclein.
We don't have any experience with mucuna pruriens. You can obtain mucuna pruriens as velvet or fava beans. It is also available in as seeds, powder, capsule or extract. The problem is finding the "dose" that works for you since much of it will be lost in the digestive process. Standardized doses may work more effectively and be safer. You can find it online as Dopabean from at least one company. Be wary of claims about the L-dopa content because many companies products are not standardized, making it very difficult to determine how much you need and to risk getting too much or too little.
9/2011 Addendum: Steve has some experience with mucuna pruriens now and we will be writing about it when he has used it for a longer period of time and we know more about the assistive benefits of EGCg found in green tea..
9/2011 Addendum: Steve has some experience with mucuna pruriens now and we will be writing about it when he has used it for a longer period of time and we know more about the assistive benefits of EGCg found in green tea..
HEALTHY DIET for PD:includes items listed above as well as below.
You're going to have to make the adjustments to your medication schedule and the type and restrictions of those meds. For nutritional suggestions, some diets like the Mediterranean diet may be a bit healthier and use some very helpful seasonings. The focus here is on olive oil which actually enables utilization of nutrients from fruits and veggetables, fish rather than too much red meat, and red wine (in moderation).
You're going to have to make the adjustments to your medication schedule and the type and restrictions of those meds. For nutritional suggestions, some diets like the Mediterranean diet may be a bit healthier and use some very helpful seasonings. The focus here is on olive oil which actually enables utilization of nutrients from fruits and veggetables, fish rather than too much red meat, and red wine (in moderation).
Is invaluable on a regular basis. This is more than our opinion it has been clinically demonstrated. If you have the $$$$ and can afford it, 2 sessions a week would be ideal. One session would be good and less than that will see many reversals of the good done. Medical massage - Swedish Massage involves the entire body with focus on the problem areas and issues and really should be done by the same licensed therapist all of the time. Massage increases endorphin levels, works to break up muscle knots, reduces stiffness and alleviates pain caused by a variety of conditions. An important element in treating postural instability, massage should be on your therapy wish list. Unfortunately this valuable therapy is not recognized by most health insurers including Medicare. Other forms of useful massage include Shiatsu/acupressure, and Neutomuscular Therapy (NMT). Massage therapy can also be beneficial as behavioral therpay when treating anxiety and depression found in PwPs...and their caregivers.
PHYSICAL THERAPY
Occupational therapy for assistance with tasks of daily living. Getting into bed, standing and sitting, buttoning a shirt, whatever. While this is not permanent on-going therapy, a patient will need refresher courses as the disease progresses. Care-givers should attend these sessions if permitted.
Exercise therapy can include a wide variety of therapies: swim, dance, yoga, tai chi, nautilus equipment, exercise bikes - especially motorized bikes for legs and arms, vocal exercises.
Forced Exercise: is a more recent concept but very exciting. If it you find access to the right equipment and can put in the required time, it might work for to reduce reliance on higher dosages of medication and to relieve some symptoms.
Voice therapy will include the very important breathing exercises to aid speaking, breathing, swallowing. If you can't get to a therapist, there are home exercises which will help.
PHYSICAL THERAPY
Occupational therapy for assistance with tasks of daily living. Getting into bed, standing and sitting, buttoning a shirt, whatever. While this is not permanent on-going therapy, a patient will need refresher courses as the disease progresses. Care-givers should attend these sessions if permitted.
Exercise therapy can include a wide variety of therapies: swim, dance, yoga, tai chi, nautilus equipment, exercise bikes - especially motorized bikes for legs and arms, vocal exercises.
Forced Exercise: is a more recent concept but very exciting. If it you find access to the right equipment and can put in the required time, it might work for to reduce reliance on higher dosages of medication and to relieve some symptoms.
Voice therapy will include the very important breathing exercises to aid speaking, breathing, swallowing. If you can't get to a therapist, there are home exercises which will help.
OTHER TREATMENTS
As the disease progresses there is also Deep Brain Stimulation if the patient meets the qualifications and the physicians feel they are good candidates.
There are older surgical procedures but are not as commonly used in this century. More treatments and surgeries are in the pipeline. However, it was announced in October, 2010 that these older surgieries are still valid and moreover can be used with DBS with the understanding that there is a higher risk of depression with subthalmic nuclei surgeries.
There are older surgical procedures but are not as commonly used in this century. More treatments and surgeries are in the pipeline. However, it was announced in October, 2010 that these older surgieries are still valid and moreover can be used with DBS with the understanding that there is a higher risk of depression with subthalmic nuclei surgeries.
While we are not convinced that any form of stem cell treatment performed now will have more than limited advantage, who wouldn't want to have that advantage for a few years? If successful, there appear to be reversals after a few years. The various forms of cell therapy are still works in progress and are still pipeline treatments.
Although not treatments, tools that can help the PD patient with activities of daily living are part of the therapy to assist unaided or semi-aided functioning. Special handled flatware, laser canes, shirts with snaps, cups that prevent spillage, walkers with baskets and seats, voice recognition programs and other computer programs to enable "typing", bath seats, higher toilet seats will be of use to many PwPs.
One last observation: a plan is needed that involves the dreaded "what if" stuff. How and who and when, where and why. Quite a bit of planning may be necessary for a disease which can render a person almost completely non-functional. Families need to discuss these matters with the patient in the beginning. Plans must be made to make the home safe for the PwP so that they can remain there as long as possible.
And plans must be made to relieve caregivers from time to time. I'd suggest weekly to be realistic to their needs. Several hours are necessary so that they can catch up with social activities, do shopping, spend some uninterrupted time with reading or email or just get a well deserved rest to make up for their own sleep deprivation.
Think what a wonderful Holiday Present some free time would be to someone who needs recharged batteries.
Think what a wonderful Holiday Present some free time would be to someone who needs recharged batteries.
Saturday, June 6, 2009
Pain and Parkinson's Disease
PD Is No Laughing Matter but Smiles and Laughter Can Help Ease the Pain
My husband has PD and I can tell you that his body aches nearly every day. As a matter of fact it was an odd sensation/pain running up his thumb that took him to the doctor for a diagnosis.
every day. As a matter of fact it was an odd sensation/pain running up his thumb that took him to the doctor for a diagnosis.
When you think about the variety of PD symptoms it is not surprising that there would be pain associated with increasing muscle stiffness. Although not everyone experiences all of the wide assortment of symptoms, as the disease progresses, probably every PWP will experience stiffness. And with the stiffness, the dystonias - the unwilled muscle contraction - comes twisting and pain, cramping and pain. But there's more.
Of interest is that even though Parkinson's disease usually begins unilaterally, pain can be bilateral. Also of interest is that men with Parkinson's have a higher perception of pain - lower pain threshold. Not by much, however. Steve's massage therapist says that the tension in the chest muscles on his bad side causes a pull and therefore pain on the good side.
The body posture of the Parkinson's shuffle can cause pain in the neck, shoulders, back, hips as the body maligns itself. Headaches are another result of this kind of pain.
PD pain can come from non-motor areas as well. There is neuropathic pain which can cause tingling, burning, numbness, sharp pain. The Parkinson's Disease Foundation breaks the causes of PD pain into five areas: Musculoskeletal, Non-Motor, Dystonia, Akathisia "discomfort due to extreme restlessness" and "a rare pain syndrome known as "primary" or "central" pain, arising from the brain." Depression can also cause and/or heighten sensitivity to pain.
Pain is not a punishment for having a disease. It is a symptom and/or a side effect and it should be addressed by you and your doctor. In some cases pain could be a side effect of medication or medication "off" times but by adjusting the dosage the pain can be lessened.
 Lowering stress levels can also reduce pain. Adjusting the body through exercise and massage therapy can make a real difference. To counteract the pain of rigidity, my husband goes to exercise therapy and gets a weekly massage specifically addressing the target points of his stiffness: his bad side shoulder, neck and left leg in the course of the full massage. In between we have small hand held massagers that really do help his neck and shoulder even when only used for a few minutes at a time. At night he uses a heated mattress pad. Electric blankets don't work as well here because dogs have an affinity for chewing them...don't ask.
Lowering stress levels can also reduce pain. Adjusting the body through exercise and massage therapy can make a real difference. To counteract the pain of rigidity, my husband goes to exercise therapy and gets a weekly massage specifically addressing the target points of his stiffness: his bad side shoulder, neck and left leg in the course of the full massage. In between we have small hand held massagers that really do help his neck and shoulder even when only used for a few minutes at a time. At night he uses a heated mattress pad. Electric blankets don't work as well here because dogs have an affinity for chewing them...don't ask.
He does his breathing and voice exercises but not as often as he should. He does those not only to be heard and understood but to avoid the panic of choking and the fear of dying that way. So he is relieving a stress producer as well.
I can't stress the importance of exercise to stretch the muscles, help the body resist the stiffness, punch up the endorphins, resist the pain. Nor can I overstress the need to warm up slowly...not to hyper-extend...because you've already got enough pain. About exercise: ease into it and then persist. You may see some results and then plateau - that doesn't mean it isn't working. Just stay at it. But mean it. Don't just go for the motions. Don't lie to yourself. Don't be an exercise potato. You actually have to work at it. Otherwise you might as well just watch a a cooking show instead of an exercise video.
There are other courses of treatment including Forced Exercise which if done properly can abate symptoms for a couple of weeks: Aqua therapy (swim therapy); Dance therapy - amazing to see PWPs leave their walkers behind to dance - Breathing and Voice therapy, and one of the best, Yoga. Yoga for movement, posture, balance, mind, flexing the right muscles to for relief of constipation, breathing, anxiety-tension relief, depression all of which aid sleeping.
Who would have suspected that the PD associated sleep disorders might actually be a contributory factor to increased pain. A cancer pain study conducted in Tennessee recently demonstrated that lack of sleep/sleep disorders may make pain worse in cancer rather than the other way around which was expected.
Successful Deep Brain Surgery can result in the reduction of both meds and symptoms. This reduction can mean a reduction of pain or the absence of pain. Permanent acupuncture can also result in a reduction of symptoms and consequently... There are other therapies in the pipeline which may seriously impact symptoms with the same pain reduction ensuing.

A few words about TENs machines (transcutaneous electrical nerve stimulation) I can't find anyone who has had success, including Steve, using one. If you have used one, we'd all like to read about your experience in the comments section.
We know that cannabinoids and cannabis components do assist with certain kinds of symptom relief as an anti-spasmodic and muscle relaxant. Parkinson's Disease is on the medical marijuana list in the states which have that understanding. In a 2004 study which involved THC, a cannabis component, demonstrated the possibility that it will help with PD pain as well as ALS spasms. At present Riluzole (the only FDA approved med for ALS) extends life from 2 - 3 months. In mouse studies, THC prolonged life for a human equivalent of 3 years or more. There are several cannabinoid receptors in the human body waiting to help with pain and stress reduction.
Laughter is a great stress reliever. If you've ever laughed with your entire body and soul, you know what I mean. You feel euphoric afterwards. Because that laugh really got your endorphins going. With those natural pain killers aroused everything else disappeared into the background for a few minutes. The smiles can come from whatever, wherever. We need them. For big smiles I go outside to watch the dogs play together. Sometime Rita picks up one of her stuffed toys just to get Harry to chase her or play tug of war...which accounts for the loose heads, limbs and stuffing around the yard. The day she "found" the dead squirrel, I quickly called a halt to that tug of war...but we were laughing anyway.
euphoric afterwards. Because that laugh really got your endorphins going. With those natural pain killers aroused everything else disappeared into the background for a few minutes. The smiles can come from whatever, wherever. We need them. For big smiles I go outside to watch the dogs play together. Sometime Rita picks up one of her stuffed toys just to get Harry to chase her or play tug of war...which accounts for the loose heads, limbs and stuffing around the yard. The day she "found" the dead squirrel, I quickly called a halt to that tug of war...but we were laughing anyway.
So when you hear people say that you need a sense of humor to have Parkinson's, they're not kidding around...or maybe they are.
references and additional reading:
http://www.pdf.org/pdf/Pain%20in%20PD.pdf
http://www.cmellc.com/geriatrictimes/g001029.html
http://en.wikipedia.org/wiki/Laughter
My husband has PD and I can tell you that his body aches nearly
 every day. As a matter of fact it was an odd sensation/pain running up his thumb that took him to the doctor for a diagnosis.
every day. As a matter of fact it was an odd sensation/pain running up his thumb that took him to the doctor for a diagnosis.When you think about the variety of PD symptoms it is not surprising that there would be pain associated with increasing muscle stiffness. Although not everyone experiences all of the wide assortment of symptoms, as the disease progresses, probably every PWP will experience stiffness. And with the stiffness, the dystonias - the unwilled muscle contraction - comes twisting and pain, cramping and pain. But there's more.
Of interest is that even though Parkinson's disease usually begins unilaterally, pain can be bilateral. Also of interest is that men with Parkinson's have a higher perception of pain - lower pain threshold. Not by much, however. Steve's massage therapist says that the tension in the chest muscles on his bad side causes a pull and therefore pain on the good side.
The body posture of the Parkinson's shuffle can cause pain in the neck, shoulders, back, hips as the body maligns itself. Headaches are another result of this kind of pain.
PD pain can come from non-motor areas as well. There is neuropathic pain which can cause tingling, burning, numbness, sharp pain. The Parkinson's Disease Foundation breaks the causes of PD pain into five areas: Musculoskeletal, Non-Motor, Dystonia, Akathisia "discomfort due to extreme restlessness" and "a rare pain syndrome known as "primary" or "central" pain, arising from the brain." Depression can also cause and/or heighten sensitivity to pain.
Pain is not a punishment for having a disease. It is a symptom and/or a side effect and it should be addressed by you and your doctor. In some cases pain could be a side effect of medication or medication "off" times but by adjusting the dosage the pain can be lessened.
 Lowering stress levels can also reduce pain. Adjusting the body through exercise and massage therapy can make a real difference. To counteract the pain of rigidity, my husband goes to exercise therapy and gets a weekly massage specifically addressing the target points of his stiffness: his bad side shoulder, neck and left leg in the course of the full massage. In between we have small hand held massagers that really do help his neck and shoulder even when only used for a few minutes at a time. At night he uses a heated mattress pad. Electric blankets don't work as well here because dogs have an affinity for chewing them...don't ask.
Lowering stress levels can also reduce pain. Adjusting the body through exercise and massage therapy can make a real difference. To counteract the pain of rigidity, my husband goes to exercise therapy and gets a weekly massage specifically addressing the target points of his stiffness: his bad side shoulder, neck and left leg in the course of the full massage. In between we have small hand held massagers that really do help his neck and shoulder even when only used for a few minutes at a time. At night he uses a heated mattress pad. Electric blankets don't work as well here because dogs have an affinity for chewing them...don't ask.He does his breathing and voice exercises but not as often as he should. He does those not only to be heard and understood but to avoid the panic of choking and the fear of dying that way. So he is relieving a stress producer as well.
I can't stress the importance of exercise to stretch the muscles, help the body resist the stiffness, punch up the endorphins, resist the pain. Nor can I overstress the need to warm up slowly...not to hyper-extend...because you've already got enough pain. About exercise: ease into it and then persist. You may see some results and then plateau - that doesn't mean it isn't working. Just stay at it. But mean it. Don't just go for the motions. Don't lie to yourself. Don't be an exercise potato. You actually have to work at it. Otherwise you might as well just watch a a cooking show instead of an exercise video.
There are other courses of treatment including Forced Exercise which if done properly can abate symptoms for a couple of weeks: Aqua therapy (swim therapy); Dance therapy - amazing to see PWPs leave their walkers behind to dance - Breathing and Voice therapy, and one of the best, Yoga. Yoga for movement, posture, balance, mind, flexing the right muscles to for relief of constipation, breathing, anxiety-tension relief, depression all of which aid sleeping.
Who would have suspected that the PD associated sleep disorders might actually be a contributory factor to increased pain. A cancer pain study conducted in Tennessee recently demonstrated that lack of sleep/sleep disorders may make pain worse in cancer rather than the other way around which was expected.
Successful Deep Brain Surgery can result in the reduction of both meds and symptoms. This reduction can mean a reduction of pain or the absence of pain. Permanent acupuncture can also result in a reduction of symptoms and consequently... There are other therapies in the pipeline which may seriously impact symptoms with the same pain reduction ensuing.

A few words about TENs machines (transcutaneous electrical nerve stimulation) I can't find anyone who has had success, including Steve, using one. If you have used one, we'd all like to read about your experience in the comments section.
We know that cannabinoids and cannabis components do assist with certain kinds of symptom relief as an anti-spasmodic and muscle relaxant. Parkinson's Disease is on the medical marijuana list in the states which have that understanding. In a 2004 study which involved THC, a cannabis component, demonstrated the possibility that it will help with PD pain as well as ALS spasms. At present Riluzole (the only FDA approved med for ALS) extends life from 2 - 3 months. In mouse studies, THC prolonged life for a human equivalent of 3 years or more. There are several cannabinoid receptors in the human body waiting to help with pain and stress reduction.
Laughter is a great stress reliever. If you've ever laughed with your entire body and soul, you know what I mean. You feel
 euphoric afterwards. Because that laugh really got your endorphins going. With those natural pain killers aroused everything else disappeared into the background for a few minutes. The smiles can come from whatever, wherever. We need them. For big smiles I go outside to watch the dogs play together. Sometime Rita picks up one of her stuffed toys just to get Harry to chase her or play tug of war...which accounts for the loose heads, limbs and stuffing around the yard. The day she "found" the dead squirrel, I quickly called a halt to that tug of war...but we were laughing anyway.
euphoric afterwards. Because that laugh really got your endorphins going. With those natural pain killers aroused everything else disappeared into the background for a few minutes. The smiles can come from whatever, wherever. We need them. For big smiles I go outside to watch the dogs play together. Sometime Rita picks up one of her stuffed toys just to get Harry to chase her or play tug of war...which accounts for the loose heads, limbs and stuffing around the yard. The day she "found" the dead squirrel, I quickly called a halt to that tug of war...but we were laughing anyway.So when you hear people say that you need a sense of humor to have Parkinson's, they're not kidding around...or maybe they are.
references and additional reading:
http://www.pdf.org/pdf/Pain%20in%20PD.pdf
http://www.cmellc.com/geriatrictimes/g001029.html
http://en.wikipedia.org/wiki/Laughter
Subscribe to:
Posts (Atom)