In the TRAP of Parkinson's disease, postural instability is the last of the big 4 symptoms. It is also the symptom which can lead to one of the leading causes of death for PD patients.
Postural instability can be caused by Parkinson's disease or can be related to syncope (fainting); orthostatic hypotension as a side effect of medications taken either for PD; neurogenic orthostatic hypotension as a result of a condition such as MSA; a cardiac condition, medication-induced dyskinesia, or another issue. Postural instability can also be a byproduct of depression for which PD does not lack.
Because there is little help through medication, that leaves devices, caregivers, exercise and the patient to recover from a fall or to better train the body to withstand the problems of postural instability.
Although I do not trust a lightweight walker for stability in heavy lifting, it might be of value if that is all that is around. It can be used for the patient to pull himself/herself up if someone is present to stabilize the walker. Otherwise both patient and walker could fall over. A cane with those extra legs at the bottom might do the job if there is arm strength.
There is also value to having handrails installed in hallways and even bathrooms just as they are on stairways. Avoiding backless chairs or stools is also advisable in order to avoid the risk of retropulsion - leaning back to regain balance or because of loss of balance with the resultant fall.
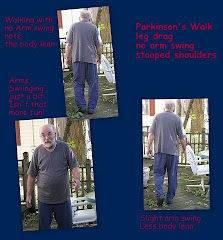
One important aid is exercise. Gait exercise can be crucial. We suggest asking for a referral to a therapy center so that gait training can be initiated. Gait training would include lengthening of stride, learning to open at the hips for a wider stance. The smaller the space between the legs, the less option to maintain balance. Lifting the legs almost in a march rather than shuffling and sticking to the floor may also be of value to provide a mental and physical cadence and to decrease the risk of the tripping on the shuffle.
Exercise addresses range of motion, flexibility stretching and yes, even strength training (to assist in rising if you do fall) and breathing. Yoga and Tai Chi exercises can help with balance and even graceful falling. Nautilus is important exercise equipment and there are less expensivel pieces of exercise equipment which can be purchased for home use. Don't neglect hand exercises. Being able to grip is crucial; a weak or claw-like hand won't help you.
Dance therapy might be helpful. Although its effects will not be physically apparent after the music stops, there might be a psychological-confidence effect which impacts postural instability due to PD depression. And it's FUN! Even in your living room. Get those endorphins going.
Locate a therapy center which has Forced Exercise equipment and aqua therapy. Water exercises can be beneficial to a PD patient because of the buoyancy effects of exercising - marching in the water. And Forced Exercise - not on a treadmill in this case unless there are trained spotters or with a support vest which attaches to the ceiling - but on the motorized exercise bicycles which compensate for the patient's inability to maintain the necessary rpms on his own. For some people these bikes are an affordable option for home use - for others, they are not. But the bike must be able to maintain between 80-90 rpm. There are two types of therapeutic bikes for this purpose. One is the Theracycle (there should be an ad link on this page). The other company is Reck MotoMed which makes several styles for home and therapy center usage.
Naturally there are aids such as shower seats (with backs or transfer seats), grab bars in the tub/shower area (no suction cups please), hand-held shower-heads with longer hoses and on-off buttons to prevent unnecessary standing in the shower. Soap on a rope.
No PD home should be without bath/shower aids even if they are not needed immediately. Knowing how to use them and using them regularly helps to train the body so that when the equipment is needed, there is kinetic memory to reinforce the use patterns. (Yes, I am a believer in the possibilities of kinetic memory to resist the tightening muscles and we have seen it work with my husband in entering/exiting the shower after the side effects of dehydration - another story - had some temporary but dire cognitive effects).
Little is available to address postural instability in PD. Usually discussed as a later PD symptom because it is apparent then, to many it is an invisible side effect as a very early symptom. Everyone talks about falls, the risks, prevention and the role they play, but we haven't found many solutions to address the problem by fixing the chemical imbalances which cause it because we are not sure precisely where in the brain the problem originates although the focus is on the brain stem.
There is one rather expensive pneumatic device which can be used in the home to aid in lifting and there appear to be patent applications for more. The link to this inflatable device is provide below at a site with which we are unfamiliar.
Have a home safety evaluation conducted. These are often done by occupational therapists - they'll survey the home, watch the patient functioning in their own environment and make safety recommendations. They need to know the patient has fallen in the past and what the ensuing problems have been.
The process for assisting a patient who has fallen is step by step after you are sure there has been no injury. Do not move an injured person. Make the call for emergency medical assistance. Or use that MedAlert button.
No injuries? Whew! Let's catch our breath. Everybody breathe calmly a few times to relax.At this point prevention and exercise seem to be the best methods to reduce the risks. Many caregivers are simply not strong enough to pull or lift a person lying on the floor without assistance. This is also another argument for the other forms of exercise accompanied by strength training.
- Encourage the patient to roll from the landing position to a prone face down position. You may be able to assist with that.
- Next the patient must raise the upper torso onto bent arms. The lower part of the arm is on the floor.
- The buttocks are next, assisted by the knees.
- With weight on the forearms, rock forward and then back as you use those abdominals to lift your butt into the air.
- The knees will walk forward and assist with the push up.
- Once the patient is on his/her knees, you can assist them if they need help. If they are unable to rise from a kneeling position, they may be able to pull up on sturdy furniture or walker. Or you may be able to brace them (their arm around your shoulders and both of you rise from a kneeling position. The caregiver must keep a straight back to avoid injury.
- If you are alone, you may be able to crawl on your knees to furniture solid enough to provide support for the pull to a standing or seated position.
additional reading:Chronic Dizziness and Postural Instability
Links to inflatable device and detailed advice on its usage:Same information if you can't view pdf format:
It's being called WiiHab and we already know that it can help with PD depression, what about postural instability? As a diagnostic it has been found to be effective:
To try the Wii at home: you'll need the Nintendo console, the balance board and some accessories such as the WiiFit program and controllers. The balance board must be on a firm surface to work properly. If balance is a serious problem, make sure you have support or supporters handy.
For more information check Wikipedia before you buy